
Home Working
There are many people working from home, given the current situation we are in with COVID-19. This percentage may drop in the future, but for now, if we can work from home, that’s what we should do.
With kitchens and spare rooms now becoming a more permanent office space for many, staff should take time to make sure the space is serving their needs and not causing any damage. Your employers can help with this in many ways. Discuss your concerns with them.
Here we look at 8 ways to improve homeworking. If you have any suggestions, let us know.
Health and safety law requires that employers do all that they can to ensure the wellbeing of their staff. This obligation has not changed due to the coronavirus pandemic, and so risks to employees need to be managed in the usual way.
Although generally low risk, homeworking is not exempt from the law, and so a risk assessment should be carried out on the home environment to identify hazards. The risk assessment will also need to establish any measures needed to prevent harm to the employee, as well as anyone else affected by their work (including other members of the household).
To assist this process, employers can remotely work through a risk assessment with members of staff or ask staff to conduct their own assessment using a template and guidance. Contact us for further information.
Managing occupational health is critical for a healthy workspace. Poor posture while working, or a lack of suitable equipment, can cause serious musculoskeletal disorders (MSD), including injuries to the back, neck, hips, knees or wrists.
With many workers converting kitchen tables and spare rooms into their new office spaces, there is a significant risk that employees could unwittingly be causing themselves long-term damage through poor seating choices or by not having the right equipment.
To ensure staff are protecting themselves from potential MSDs, employers should try to find out about their staff’s working conditions and check that everyone knows how to set up their workspace. As a minimum, the risk assessment will likely identify that everyone needs carry out a display screen equipment (DSE) check and know how to report any problems.
Search through our previous blogs for DSE information.
As well as sitting correctly, moving is also an important part of maintaining good musculoskeletal health. In the typical office, people are much more likely to have situations where they need to walk around — as part of their commute, to go to a meeting, or to speak to a colleague. Many of these workplace opportunities to stretch the legs have now been lost, so as well as taking breaks from looking at a screen (as required by the DSE Regulations) encourage staff to take a regular breather to get up and move around. Setting a timer on a phone can be a relatively easy way to do this.
Routine is important to help protect mental health and to provide continuity in the working day. Having clear start and finish times helps create work–life boundaries, as can creating a dedicated workspace.
Wherever possible, ask staff to mix up their to-do list to create balance in their work. Spending all day in video conferences can be extremely fatiguing, as can hours in front of a screen with no workplace contact at all. When evaluating new working arrangements, also ask staff to consider how they are finding the new methods of working.
Working from home brings additional cyber security issues that organisations may not have considered. The National Cyber Security Centre provides comprehensive advice on what employers might need to think about, but a starting point would be to check that staff:
If the organisation has any e-learning modules that cover cyber security, then consider asking all staff to carry out refresher training.
House fires are much more likely to occur when people are at home. When considering the home office, ways to prevent fires include:
Employees working from home should also check that they have working smoke alarms that are tested once a week.
Working from home might mean using new technology. Whereas some may find this an easy transition, others may find it harder. It is commonplace for staff to have previously asked nearby colleagues for help with IT issues, so check in to ask if there are any problems.
Working from home will bring additional costs, e.g. to keep the workspace warm. To help keep energy costs low, organisations could raise awareness of energy efficiency measures that staff can adopt. Some examples might include:
Contact us should you require further information.
Keep safe!

Health and Safety Law
Everyone’s business experiences a health and safety problem at some point.
The list of possibilities for workplace injury, illness, or even death might be endless.
Slips and trips, burns, gas, spillages, asbestos, structural collapses, tight spaces, strains. We could sit here all day and list the many ways that you or one of your employees or colleagues could suffer at work.
But instead, how about we go through the ways that you can make sure that your staff are aware of and adhere to your company’s health and safety policy?
In many instances below–what applies to your staff might also apply to visitors, contractors, and any other persons who could be affected by your health and safety policies.
The Health and Safety at Work Act 1974 does outline the responsibilities that an employer like you has for the health & safety of their staff while they’re working for you.
Health and safety is, for many, a chore. It involves paperwork, it sounds boring, and it isn’t pleasant. So a week’s worth of policy reading about health & safety isn’t going to look persuasive to anyone in your employ.
Provide up-to-date information that is written simplistically so everyone can follow it. The information should include:
Written copies.
Think email. Think white papers. Think employee/company handbooks. Think specific policy folders in the filing cabinets at the back of the office. Or, if you’ve gone paperless, on your company’s intranet/storage cloud. Then, once you’ve made and stored said policies, send them to your staff. Make access as easy as possible.
If you’ve made your staff aware of your policies and procedures, you’ll probably have a better defence if someone takes you to an employment tribunal if they suffer an injury.
It never hurts anyone to put your employees through their health & safety training paces. Whether you’ve got a team of veteran engineers or junior salespeople, you want all staff to have a minimum level of training, that is, ideally, state-of-the-art.
To do this, you could invite health & safety specialists to your workplace to give talks, hold training exercises, lead discussions, and then even invigilate assessments. If you want to ensure people are learning what they’re being taught, what better proof than an assessment at the end? We all yearn for those long-gone days of exam revision after all, don’t we?
Additional resources such as web-based tools, videos, case studies and incentives such rewarding your employees with a salary review can all be effective methods for helping your employees to learn about how they follow your company’s health & safety policy.
Whether it’s hard hats, masks, safety footwear, jackets, hivis vests – make it available for your staff.
Once you’ve done this, run an instructional course on how to correctly use and maintain all equipment, and if you want to be really thorough again, put your staff through another assessment.
You know the drill. If the floor is wet, get out the yellow sign.
If your workplace bears any significant risk that cannot be avoided or control in another way, ensure there is a sign to inform staff, thus lowering the risk of injury.
Ensure you have the correct cover and resources during the COVID-19 pandemic. Stock your first aid kit and ensure that everyone knows who the first aider(s) is. You should assess (regularly) your first aid situation. If your company is growing exponentially, you might need to add personnel to your first aid team.
Contact us for further information.
Guest Blogger – Kate Palmer

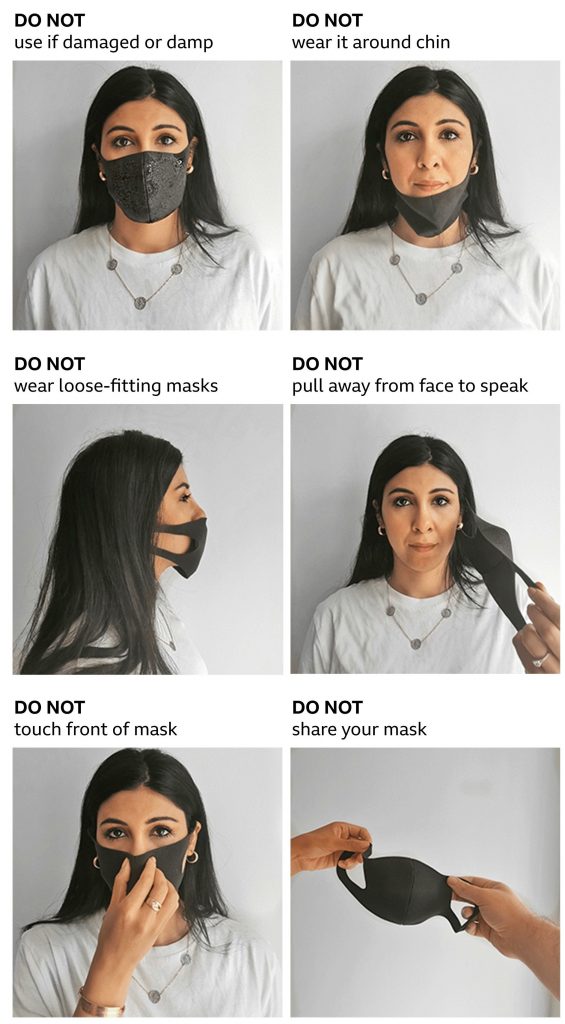
How not to wear a face covering or mask
The coronavirus is here for the long haul! The future will depend on social mixing and the prevention that we have in place and how we comply with that.
Wash your hands often – if soap and water are not readily available, use a hand sanitizer that contains at least 60% alcohol. Cover all surfaces of your hands and rub them together until they feel dry.
Avoid close contact – everyone should wear a mask in public settings and when around people who don’t live in your household.
Clean and disinfect – clean and disinfect frequently touched surfaces daily. This includes tables, doorknobs, light switches, countertops, handles, desks, phones, keyboards, toilets, faucets, and sinks.
Monitor Your Health Daily – be alert for symptoms. Watch for fever, cough, shortness of breath, or other symptoms of COVID-19.
Face coverings must be worn by customers in shops, supermarkets and shopping centres. Shop workers will now also have to wear a face covering.
Face coverings are compulsory for anyone travelling by public transport in England, Scotland and Wales, unless they have an exemption or a reasonable excuse. People can be refused travel if they do not follow the rules and can be fined as a last resort.
Face coverings are also compulsory in a number of indoor spaces. These include:
Some people do not have to wear a face covering. They include:
You can take off your mask if:
World Health Organization (WHO) advice says non-medical face coverings should be worn in public where social distancing is not possible.
Coronavirus is spread when droplets are sprayed into the air when infected people talk, cough or sneeze. Those droplets can then fall on surfaces.
The WHO says there is also emerging evidence of airborne transmission of the virus, with tiny particles hanging in aerosol form in the air.
Homemade cloth face coverings can help reduce the spread from people who are contagious but have no symptoms or are yet to develop symptoms. Taking a face covering on and off can also risk contamination, the WHO says.
Contact us if you require further information.
Thank you to Royal Devon and Exeter NHS Foundation Trust for the mask infographic.
Information correct at time of publishing.

First Aid Cover During Reduced Staffing as a Result of Covid-19
If first-aid cover for your business is reduced because of coronavirus (perhaps your first aiders are furloughed or working from home) or you can’t get the first-aid training you need, there are some things you can do so that you still comply with the law.
You should review your first aid needs assessment and decide if you can still provide the cover needed for the workers that are present and the activities that they are doing.
If there are fewer people coming into your workplace, it may still be safe to operate with reduced first-aid cover. You could also stop higher risk activities.
You could share the first aiders of another business, but be sure that they have the knowledge, experience and availability to cover the first aid needs of your business.
Shared first aiders must:
Whoever provides the temporary cover must make sure they do not adversely affect their own first-aid cover.
If your first aiders hold a first-aid certificate that expires on or after 16 March 2020 and have not been able to access requalification training because of coronavirus, they may qualify for a three-month extension. This applies to the following courses:
To qualify for the extension, you must be able to explain why they have not been able to requalify and demonstrate what steps you have taken to access the training, if asked to do so.
Courses are now available for requalification. In England, the final deadline for requalification for these qualifications is 30 September 2020. There is no deadline yet for Scotland and Wales, but employers or certificate holders are encouraged to arrange requalification training as soon as they can.
There are also online options for first aid training. We use a company called IHASCO. Contact them by clicking here.
Contact us should you require further information.

Workplace inspections help prevent injuries and illnesses while promoting safe working. Through critical examination of the workplace, inspections identify and record hazards for corrective action. Joint occupational health and safety committees plan, conduct, report and monitor inspections. Regular workplace inspections are an important part of the overall occupational health and safety program.
As an essential part of a health and safety program, a company should examine the workplace to:
Look at all workplace elements – the environment, the equipment and the process. The environment includes such hazards as noise, vibration, lighting, temperature, and ventilation. Equipment includes materials, tools and apparatus for producing a product or a service. The process involves how the worker interacts with the other elements in a series of tasks or operations.
Types of workplace hazards include:
Inspection records are important. Past inspection records show what inspectors identified. They also show what an inspection team concentrated on and what areas it did not inspect.
The inspection report can draw attention to possible hazards. However, do not simply repeat or copy previous inspections. Check the inspection report to confirm implementation of previous recommendations.
The following describes three other types of inspection reports:
Supervisors and workers repeatedly conduct ongoing inspections as part of their job responsibilities. Such inspections identify hazardous conditions and either correct them immediately or report them for corrective action. The frequency of these inspections varies with the amount and conditions of equipment use. Daily checks by users assure that the equipment meets minimum acceptable safety requirements.
Pre-operation checks involve inspections of new or modified equipment or processes. Workers often perform these after workplace shutdowns.
Periodic inspections are regular, planned checks of critical equipment or system components. These components have a high potential for causing serious injury or illness. The inspections are often part of preventive maintenance procedures or hazard control programs.
The law specifies that qualified persons inspect some types of equipment on a recurring basis. This includes elevators, boilers, pressure vessels, and fire extinguishers, at regular intervals.
The health and safety committee should review the progress of the recommendations. This is especially important when they pertain to the education and training of employees. It is also the committee’s responsibility to study the information from regular inspections. This will help in identifying trends for the maintenance of an effective health and safety program.
If you require further information please contact us.